What Parameter Does An Ehr Consider To Find Information On Service-specific Data?

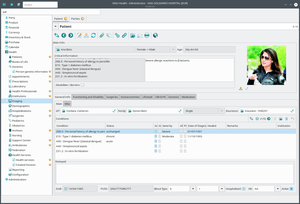
Sample view of an electronic health tape
An electronic health record (EHR) is the systematized collection of patient and population electronically stored wellness information in a digital format.[i] These records can be shared across dissimilar health intendance settings. Records are shared through network-connected, enterprise-broad information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics similar age and weight, and billing data.[2]
For several decades, electronic health records (EHRs) accept been touted every bit primal to increasing of quality intendance.[iii] Electronic wellness records are used for other reasons than charting for patients;[4] today, providers are using data from patient records to improve quality outcomes through their care management programs. EHR combines all patients demographics into a large pool, and uses this information to assist with the creation of "new treatments or innovation in healthcare delivery" which overall improves the goals in healthcare.[5] Combining multiple types of clinical data from the arrangement's wellness records has helped clinicians identify and stratify chronically sick patients. EHR can improve quality care by using the data and analytics to prevent hospitalizations among high-gamble patients.
EHR systems are designed to store information accurately and to capture the state of a patient across time. It eliminates the need to track down a patient's previous newspaper medical records and assists in ensuring data is upward-to-date,[6] accurate and legible. It also allows open up communication between the patient and the provider, while providing "privacy and security."[half dozen] It can reduce run a risk of data replication as there is only one modifiable file, which means the file is more likely up to appointment and decreases chance of lost paperwork and is cost efficient.[half dozen] Due to the digital information being searchable and in a single file, EMRs (electronic medical records) are more effective when extracting medical information for the examination of possible trends and long term changes in a patient. Population-based studies of medical records may likewise be facilitated by the widespread adoption of EHRs and EMRs.
Terminology [edit]
The terms EHR, electronic patient record (EPR) and EMR have oftentimes been used interchangeably, merely differences between the models are at present existence defined. The electronic health tape (EHR) is a more longitudinal collection of the electronic wellness information of individual patients or populations. The EMR, in contrast, is the patient record created past providers for specific encounters in hospitals and ambulatory environments and can serve as a data source for an EHR.[vii] [8]
In contrast, a personal wellness record (PHR) is an electronic application for recording personal medical information that the individual patient controls and may make available to health providers.[9]
Comparing with newspaper-based records [edit]
While in that location is still a considerable amount of fence around the superiority of electronic health records over paper records, the inquiry literature paints a more realistic picture of the benefits and downsides.[ten]
The increased transparency, portability, and accessibility acquired by the adoption of electronic medical records may increase the ease with which they can be accessed by healthcare professionals, but too tin increase the amount of stolen information past unauthorized persons or unscrupulous users versus newspaper medical records, as acknowledged by the increased security requirements for electronic medical records included in the Health Information and Accessibility Human activity and by large-calibration breaches in confidential records reported by EMR users.[11] [12] Concerns nigh security contribute to the resistance shown to their adoption.[ weasel words ] When users log in into the electronic wellness records, it is their responsibility to make sure the information stays confidential and this is done by keeping their passwords unknown to others and logging off before leaving the station.[13]
Handwritten paper medical records may be poorly legible, which can contribute to medical errors.[14] Pre-printed forms, standardization of abbreviations and standards for penmanship were encouraged to meliorate the reliability of paper medical records. An example of possible medical errors is the assistants of medication. Medication is an intervention that can plough a person's condition from stable to unstable very quickly. With paper documentation it is very easy to not properly document the administration of medication, the time given, or errors such as giving the "wrong drug, dose, form, or non checking for allergies" and could affect the patient negatively. It has been reported that these errors have been reduced by "55-83%" because records are at present online and require certain steps to avoid these errors.[15]
Electronic records may assistance with the standardization of forms, terminology, and information input.[16] Digitization of forms facilitates the collection of information for epidemiology and clinical studies.[17] [xviii] All the same, standardization may create challenges for local practice.[10] Overall, those with EMRs that have automated notes and records, order entry, and clinical decision support had fewer complications, lower mortality rates, and lower costs.[19]
EMRs tin can be continuously updated (inside certain legal limitations: see below). If the power to exchange records between dissimilar EMR systems were perfected ("interoperability"[xx]), it would facilitate the coordination of health care delivery in nonaffiliated wellness care facilities. In addition, data from an electronic system can be used anonymously for statistical reporting in matters such as quality improvement, resource direction, and public health catching disease surveillance.[21] However, it is difficult to remove data from its context.[10]
Usefulness for inquiry [edit]
Electronic medical records could as well be studied to quantify disease burdens – such every bit the number of deaths from antimicrobial resistance[22] – or aid place causes of, factors of and contributors to diseases,[23] [24] peculiarly when combined with genome-broad association studies.[25] [26] For such purposes, electronic medical records could potentially be fabricated available in securely anonymized or pseudonymized[27] forms to ensure patients' privacy is maintained.[28] [26] [29] [30] This may enable increased flexibility, improved affliction surveillance, and novel life-saving treatments.
GNU Health patient main screen as of 2013
Theoretically, gratuitous software such equally GNU Health could be used or modified for various purposes that employ electronic medical records i.a. via securely sharing anonymized patient treatments, medical history and private outcomes (including past common primary care physicians).[31]
Emergency medical services [edit]
Ambulance services in Commonwealth of australia, the United States and the U.k. have introduced the use of EMR systems.[32] [33] EMS Encounters in the U.s. are recorded using various platforms and vendors in compliance with the NEMSIS (National European monetary system Information Organization) standard.[34] The benefits of electronic records in ambulances include: patient data sharing, injury/illness prevention, better preparation for paramedics, review of clinical standards, amend research options for pre-hospital care and pattern of future treatment options, data based event improvement, and clinical decision support.[35]
Technical features [edit]
- Digital formatting enables data to be used and shared over secure networks
- Track care (e.one thousand. prescriptions) and outcomes (e.yard. blood pressure)
- Trigger warnings and reminders
- Transport and receive orders, reports, and results
- Decrease billing processing time and create more accurate billing system
Wellness Data Commutation[36]
- Technical and social framework that enables information to move electronically betwixt organizations
Using an EMR to read and write a patient'south record is not only possible through a workstation but, depending on the type of arrangement and wellness care settings, may as well be possible through mobile devices that are handwriting capable,[37] tablets and smartphones. Electronic Medical Records may include access to Personal Health Records (PHR) which makes individual notes from an EMR readily visible and accessible for consumers.[ commendation needed ]
Some EMR systems automatically monitor clinical events, by analyzing patient information from an electronic health record to predict, observe and potentially forbid adverse events. This tin include discharge/transfer orders, pharmacy orders, radiology results, laboratory results and whatsoever other information from ancillary services or provider notes.[38] This blazon of event monitoring has been implemented using the Louisiana Public health information exchange linking statewide public health with electronic medical records. This organization alerted medical providers when a patient with HIV/AIDS had non received intendance in over twelve months. This system greatly reduced the number of missed disquisitional opportunities.[39]
Philosophical views [edit]
Inside a meta-narrative systematic review of enquiry in the field, diverse different philosophical approaches to the EHR exist.[40] The health data systems literature has seen the EHR as a container property data about the patient, and a tool for aggregating clinical data for secondary uses (billing, audit, etc.). However, other enquiry traditions see the EHR equally a contextualised artifact within a socio-technical organization. For example, actor-network theory would see the EHR as an actant in a network,[41] and research in computer supported cooperative piece of work (CSCW) sees the EHR as a tool supporting particular work.
Several possible advantages to EHRs over newspaper records have been proposed, but there is debate about the degree to which these are accomplished in practice.[42]
Implementation [edit]
Quality [edit]
Several studies call into question whether EHRs improve the quality of intendance.[40] [43] [44] [45] [46] One 2011 study in diabetes intendance, published in the New England Journal of Medicine, found evidence that practices with EHR provided amend quality intendance.[47]
EMRs may eventually help improve care coordination. An article in a merchandise periodical suggests that since anyone using an EMR can view the patient'southward full chart, information technology cuts down on guessing histories, seeing multiple specialists, smooths transitions between care settings, and may allow ameliorate intendance in emergency situations.[48] EHRs may also improve prevention by providing doctors and patients better access to exam results, identifying missing patient information, and offer evidence-based recommendations for preventive services.[49]
Costs [edit]
The steep price of EHR and provider uncertainty regarding the value they will derive from adoption in the form of return on investment has a significant influence on EHR adoption.[l] In a project initiated by the Role of the National Coordinator for Health Information (ONC), surveyors found that infirmary administrators and physicians who had adopted EHR noted that any gains in efficiency were offset past reduced productivity as the technology was implemented, besides as the demand to increase it staff to maintain the system.[50]
The U.S. Congressional Budget Function concluded that the cost savings may occur simply in large integrated institutions like Kaiser Permanente, and not in small doc offices. They challenged the Rand Corporation's estimates of savings. "Office-based physicians in particular may run across no benefit if they purchase such a production—and may even suffer financial impairment. Even though the use of health IT could generate price savings for the wellness system at large that might offset the EHR's cost, many physicians might not be able to reduce their office expenses or increase their revenue sufficiently to pay for it. For example, the use of health IT could reduce the number of duplicated diagnostic tests. However, that comeback in efficiency would be unlikely to increment the income of many physicians."[51] One CEO of an EHR company has argued if a physician performs tests in the function, it might reduce his or her income.[52]
Doubts have been raised about cost saving from EHRs by researchers at Harvard University, the Wharton School of the Academy of Pennsylvania, Stanford Academy, and others.[46] [53] [54]
Fourth dimension [edit]
The implementation of EMR can potentially subtract identification time of patients upon hospital access. A inquiry from the Annals of Internal Medicine showed that since the adoption of EMR a relative decrease in time by 65% has been recorded (from 130 to 46 hours).[55]
Software quality and usability deficiencies [edit]
The Healthcare Information and Management Systems Society, a very big U.S. healthcare It industry merchandise group, observed in 2009 that EHR adoption rates "accept been slower than expected in the The states, specially in comparison to other industry sectors and other adult countries. A fundamental reason, aside from initial costs and lost productivity during EMR implementation, is lack of efficiency and usability of EMRs currently available."[56] [57] The U.Southward. National Establish of Standards and Technology of the Department of Commerce studied usability in 2011 and lists a number of specific problems that have been reported past health intendance workers.[58] The U.Southward. military's EHR, AHLTA, was reported to have pregnant usability issues.[59] Furthermore, studies such as the one conducted in BMC Medical Information science and Decision Making, besides showed that although the implementation of electronic medical records systems has been a great help to general practitioners there is yet much room for revision in the overall framework and the amount of preparation provided.[threescore] It was observed that the efforts to improve EHR usability should be placed in the context of physician-patient communication.[61]
Nevertheless, physicians are embracing mobile technologies such as smartphones and tablets at a rapid footstep. Co-ordinate to a 2012 survey by Physicians Practice, 62.half dozen percent of respondents (1,369 physicians, practise managers, and other healthcare providers) say they use mobile devices in the performance of their job. Mobile devices are increasingly able to sync upwardly with electronic health record systems thus allowing physicians to access patient records from remote locations. Near devices are extensions of desk-bound-top EHR systems, using a diverseness of software to communicate and access files remotely. The advantages of instant access to patient records at any time and whatever place are clear, just bring a host of security concerns. Every bit mobile systems go more prevalent, practices will demand comprehensive policies that govern security measures and patient privacy regulations.[62]
Other advanced computational techniques have allowed EHRs to exist evaluated at a much quicker rate. Natural language processing is increasingly used to search EMRs, specially through searching and analyzing notes and text that would otherwise be inaccessible for study when seeking to improve care.[63] One report found that several machine learning methods could be used to predict the rate of a patient's mortality with moderate success, with the most successful approach including using a combination of a convolutional neural network and a heterogenous graph model.[64]
Hardware and workflow considerations [edit]
When a health facility has documented their workflow and chosen their software solution they must then consider the hardware and supporting device infrastructure for the end users. Staff and patients will need to engage with diverse devices throughout a patient's stay and charting workflow. Computers, laptops, all-in-one computers, tablets, mouse, keyboards and monitors are all hardware devices that may exist utilized. Other considerations volition include supporting work surfaces and equipment, wall desks or articulating artillery for end users to work on. Another important factor is how all these devices will be physically secured and how they will be charged that staff can always utilize the devices for EHR charting when needed.
The success of eHealth interventions is largely dependent on the power of the adopter to fully understand workflow and anticipate potential clinical processes prior to implementations. Failure to practise and so can create plush and time-consuming interruptions to service delivery.[65]
Unintended consequences [edit]
Per empirical research in social informatics, information and communications technology (ICT) apply can pb to both intended and unintended consequences.[66] [67] [68]
A 2008 Sentinel Event Alert from the U.S. Joint Committee, the organization that accredits American hospitals to provide healthcare services, states, 'As wellness it (Striking) and 'converging technologies'—the interrelationship between medical devices and Hitting—are increasingly adopted past health care organizations, users must be mindful of the safety risks and preventable agin events that these implementations tin can create or perpetuate. Technology-related agin events can be associated with all components of a comprehensive technology arrangement and may involve errors of either committee or omission. These unintended adverse events typically stem from man-machine interfaces or organization/system blueprint."[69] The Articulation Commission cites every bit an case the United states Pharmacopeia MEDMARX database[70] where of 176,409 medication error records for 2006, approximately 25 percent (43,372) involved some aspect of computer engineering as at to the lowest degree one crusade of the fault.
The British National Health Service (NHS) reports specific examples of potential and actual EHR-caused unintended consequences in its 2009 document on the management of clinical risk relating to the deployment and use of wellness software.[71]
In a February 2010, an American Food and Drug Assistants (FDA) memorandum noted that EHR unintended consequences include EHR-related medical errors from (1) errors of committee (EOC), (2) errors of omission or manual (EOT), (3) errors in information analysis (EDA), and (4) incompatibility between multi-vendor software applications or systems (ISMA), examples were cited. The FDA too noted that the "absence of mandatory reporting enforcement of H-IT safe issues limits the numbers of medical device reports (MDRs) and impedes a more comprehensive understanding of the actual problems and implications."[72]
A 2010 Lath Position Paper by the American Medical Information science Association (AMIA) contains recommendations on EHR-related patient safe, transparency, ethics education for purchasers and users, adoption of best practices, and re-examination of regulation of electronic wellness applications.[73] Beyond physical issues such every bit conflicts of involvement and privacy concerns, questions have been raised nigh the means in which the physician-patient relationship would exist affected by an electronic intermediary.[74] [75]
During the implementation phase, cognitive workload for healthcare professionals may be significantly increased as they get familiar with a new system.[76]
EHRs are almost invariably detrimental to doctor productivity, whether the data is entered during the encounter or sometime thereafter.[77] It is possible for an EHR to increase physician productivity by providing a fast and intuitive interface for viewing and understanding patient clinical data and minimizing the number of clinically-irrelevant questions,[ citation needed ] simply that is nigh never the case.[ citation needed ] The other manner to mitigate the detriment to physician productivity is to rent scribes to work aslope medical practitioners, which is most never financially feasible.[ commendation needed ]
Equally a result, many have conducted studies like the one discussed in the Journal of the American Medical Informatics Association, "The Extent And Importance of Unintended Consequences Related To Computerized Provider Order Entry," which seeks to empathize the degree and significance of unplanned adverse consequences related to computerized physician order entry and understand how to interpret adverse events and sympathise the importance of its management for the overall success of computer physician order entry.[78]
Governance, privacy and legal issues [edit]
Privacy concerns [edit]
In the U.s.a., Great Britain, and Germany, the concept of a national centralized server model of healthcare data has been poorly received.[79] Issues of privacy and security in such a model have been of concern.[fourscore] [81]
In the European Union (Eu), a new direct-binding instrument, a regulation of the European Parliament and of the council, was passed in 2016 to get into upshot in 2018 to protect the processing of personal information, including that for purposes of health care, the General Data Protection Regulation.
Threats to health care information tin can be categorized nether three headings:
- Man threats, such as employees or hackers
- Natural and environmental threats, such equally earthquakes, hurricanes and fires.
- Engineering failures, such as a system crashing
These threats tin can either be internal, external, intentional and unintentional. Therefore, one will find health data systems professionals having these particular threats in mind when discussing means to protect the health information of patients. Information technology has been found that there is a lack of security awareness among health care professionals in countries such equally Kingdom of spain.[82] The Health Insurance Portability and Accountability Act (HIPAA) has developed a framework to mitigate the harm of these threats that is comprehensive but not so specific every bit to limit the options of healthcare professionals who may accept access to different technology.[83]
Personal Data Protection and Electronic Documents Act (PIPEDA) was given Royal Assent in Canada on thirteen April 2000 to found rules on the use, disclosure and collection of personal information. The personal information includes both non-digital and electronic form. In 2002, PIPEDA extended to the health sector in Stage 2 of the law'southward implementation.[84] There are four provinces where this police does not apply because its privacy police was considered similar to PIPEDA: Alberta, British Columbia, Ontario and Quebec.
The COVID-19 pandemic in the United Kingdom led to radical changes. NHS Digital and NHSX made changes, said to be just for the elapsing of the crisis, to the information sharing organisation GP Connect across England, meaning that patient records are shared across principal care. Only patients who have specifically opted out are excluded.[85]
Legal issues [edit]
Liability [edit]
Legal liability in all aspects of healthcare was an increasing problem in the 1990s and 2000s. The surge in the per capita number of attorneys in the USA[86] and changes in the tort system acquired an increase in the toll of every attribute of healthcare, and healthcare engineering science was no exception.[87]
Failure or damages caused during installation or utilization of an EHR organisation has been feared as a threat in lawsuits.[88] Similarly, it's of import to recognize that the implementation of electronic health records carries with it pregnant legal risks.[89]
This liability business organisation was of special concern for modest EHR arrangement makers. Some smaller companies may be forced to carelessness markets based on the regional liability climate.[90] [ unreliable source ] Larger EHR providers (or regime-sponsored providers of EHRs) are amend able to withstand legal assaults.
While there is no argument that electronic documentation of patient visits and information brings improved patient intendance, there is increasing concern that such documentation could open physicians to an increased incidence of malpractice suits. Disabling physician alerts, selecting from dropdown menus, and the use of templates can encourage physicians to skip a consummate review of by patient history and medications, and thus miss of import data.
Another potential problem is electronic fourth dimension stamps. Many physicians are unaware that EHR systems produce an electronic time stamp every time the patient record is updated. If a malpractice merits goes to court, through the process of discovery, the prosecution tin can request a detailed record of all entries fabricated in a patient's electronic record. Waiting to chart patient notes until the end of the day and making addendums to records well afterwards the patient visit tin be problematic, in that this practice could result in less than accurate patient data or signal possible intent to illegally alter the patient'southward tape.[91]
In some communities, hospitals endeavour to standardize EHR systems by providing discounted versions of the hospital's software to local healthcare providers. A challenge to this do has been raised as being a violation of Stark rules that prohibit hospitals from preferentially profitable community healthcare providers.[92] In 2006, however, exceptions to the Stark rule were enacted to permit hospitals to furnish software and preparation to community providers, mostly removing this legal obstacle.[93] [ unreliable source ] [94] [ unreliable source ]
Legal interoperability [edit]
In cross-border utilize cases of EHR implementations, the boosted event of legal interoperability arises. Different countries may accept diverging legal requirements for the content or usage of electronic wellness records, which can require radical changes to the technical makeup of the EHR implementation in question. (especially when fundamental legal incompatibilities are involved) Exploring these issues is therefore frequently necessary when implementing cross-border EHR solutions.[95]
Contribution under United nations assistants and accredited organizations [edit]
The United Nations World Health Organization (WHO) administration intentionally does non contribute to an internationally standardized view of medical records nor to personal health records. However, WHO contributes to minimum requirements definition for developing countries.[96]
The United Nations accredited standardization torso International Organization for Standardization (ISO) withal has settled thorough word[ clarification needed ] for standards in the scope of the HL7 platform for wellness care computer science. Respective standards are available with ISO/HL7 10781:2009 Electronic Wellness Record-System Functional Model, Release i.1[97] and subsequent prepare of detailing standards.[98]
Medical data breach [edit]
The majority of the countries in Europe have fabricated a strategy for the development and implementation of the Electronic Health Record Systems. This would hateful greater access to health records by numerous stakeholders, even from countries with lower levels of privacy protection. The forthcoming implementation of the Cross Border Health Directive and the Eu Committee's plans to centralize all wellness records are of prime concern to the Eu public who believe that the health intendance organizations and governments cannot be trusted to manage their data electronically and expose them to more than threats.
The idea of a centralized electronic health record system was poorly received past the public who are wary that governments may use of the organization beyond its intended purpose. In that location is likewise the risk for privacy breaches that could allow sensitive wellness care information to autumn into the incorrect hands. Some countries accept enacted laws requiring safeguards to be put in identify to protect the security and confidentiality of medical information. These safeguards add protection for records that are shared electronically and give patients some important rights to monitor their medical records and receive notification for loss and unauthorized acquisition of health information. The U.s.a. and the European union have imposed mandatory medical information breach notifications.[99]
Breach notification [edit]
The purpose of a personal data breach notification is to protect individuals so that they tin have all the necessary actions to limit the undesirable furnishings of the breach and to motivate the organization to amend the security of the infrastructure to protect the confidentiality of the data. The U.s. law requires the entities to inform the individuals in the event of alienation while the EU Directive currently requires breach notification merely when the breach is probable to adversely impact the privacy of the individual. Personal health data is valuable to individuals and is therefore difficult to make an assessment whether the breach will cause reputational or financial harm or cause adverse effects on i's privacy.
The Alienation notification police in the EU provides better privacy safeguards with fewer exemptions, dissimilar the US law which exempts unintentional acquisition, access, or use of protected health information and inadvertent disclosure under a good faith conventionalities.[99]
Technical issues [edit]
Standards [edit]
- ASC X12 (EDI) – transaction protocols used for transmitting patient information. Popular in the United states for transmission of billing data.
- CEN's TC/251 provides EHR standards in Europe including:
- EN 13606, communication standards for EHR information
- CONTSYS (EN 13940), supports continuity of intendance record standardization.
- HISA (EN 12967), a services standard for inter-system communication in a clinical information environment.
- Continuity of Care Record – ASTM International Continuity of Intendance Tape standard
- DICOM – an international communications protocol standard for representing and transmitting radiology (and other) image-based data, sponsored by NEMA (National Electric Manufacturers Association)
- HL7 (HL7v2, C-CDA) – a standardized messaging and text communications protocol between hospital and md record systems, and between practice management systems
- Fast Healthcare Interoperability Resources (FHIR) – a modernized proposal from HL7 designed to provide open, granular access to medical information
- ISO – ISO TC 215 provides international technical specifications for EHRs. ISO 18308 describes EHR architectures
- xDT – a family of information commutation formats for medical purposes that is used in the German public wellness system.
The U.S. federal government has issued new rules of electronic wellness records.[100]
Open up specifications [edit]
- openEHR: an open community adult specification for a shared health record with web-based content developed online by experts. Potent multilingual adequacy.
- Virtual Medical Record: HL7's proposed model for interfacing with clinical decision support systems.
- SMART (Substitutable Medical Apps, reusable technologies): an open up platform specification to provide a standard base for healthcare applications.[101]
Common data model (in health data context) [edit]
A common data model (CDM) is a specification that describes how data from multiple sources (east.g., multiple EHR systems) can be combined. Many CDMs use a relational model (e.g., the OMOP CDM). A relational CDM defines names of tables and table columns and restricts what values are valid.
- Sentinel Common Data Model: Initially started as Mini-Lookout in 2008. Apply by the Sentinel Initiative of the USA's Nutrient and Drug Administration.
- OMOP Common Information Model: model that defines how electronic health record data, medical billing information or other healthcare data from multiple institutions tin exist harmonized and queried in unified way. Information technology is maintained by Observational Health Data Sciences and Computer science consortium.
- PCORNet Common Data Model: Kickoff defined in 2014 and used by PCORI and People-Centered Research Foundation.
- Virtual Data Warehouse: First divers in 2006 by HMO Inquiry Network. Since 2015, by Wellness Intendance System Research Network.
Customization [edit]
Each healthcare environs functions differently, frequently in significant ways. It is difficult to create a "ane-size-fits-all" EHR system. Many first generation EHRs were designed to fit the needs of primary intendance physicians, leaving certain specialties significantly less satisfied with their EHR organization.[ commendation needed ]
An ideal EHR organization volition have record standardization but interfaces that tin be customized to each provider surround. Modularity in an EHR system facilitates this. Many EHR companies employ vendors to provide customization.
This customization tin ofttimes exist washed so that a doctor's input interface closely mimics previously utilized paper forms.[102]
At the same fourth dimension they reported negative effects in communication, increased overtime, and missing records when a not-customized EMR system was utilized.[103] Customizing the software when information technology is released yields the highest benefits because it is adjusted for the users and tailored to workflows specific to the institution.[104]
Customization can have its disadvantages. At that place is, of form, higher costs involved to implementation of a customized system initially. More time must be spent past both the implementation team and the healthcare provider to empathize the workflow needs.
Development and maintenance of these interfaces and customizations tin can too lead to higher software implementation and maintenance costs.[105] [ unreliable source ] [106] [ unreliable source ]
Long-term preservation and storage of records [edit]
An important consideration in the process of developing electronic health records is to plan for the long-term preservation and storage of these records. The field will need to come to consensus on the length of time to store EHRs, methods to ensure the future accessibility and compatibility of archived data with yethoped-for developed retrieval systems, and how to ensure the physical and virtual security of the archives.[ citation needed ]
Additionally, considerations nearly long-term storage of electronic health records are complicated by the possibility that the records might one day be used longitudinally and integrated beyond sites of care. Records have the potential to exist created, used, edited, and viewed by multiple independent entities. These entities include, just are not limited to, principal intendance physicians, hospitals, insurance companies, and patients. Mandl et al. accept noted that "choices near the structure and buying of these records volition have profound impact on the accessibility and privacy of patient information."[107]
The required length of storage of an private electronic health record will depend on national and state regulations, which are subject area to alter over time.[108] Ruotsalainen and Manning have found that the typical preservation time of patient data varies betwixt 20 and 100 years. In one case of how an EHR archive might function, their research "describes a co-operative trusted notary archive (TNA) which receives wellness data from dissimilar EHR-systems, stores information together with associated meta-information for long periods and distributes EHR-information objects. TNA tin can store objects in XML-format and show the integrity of stored data with the help of event records, timestamps and annal due east-signatures."[109]
In addition to the TNA archive described by Ruotsalainen and Manning, other combinations of EHR systems and annal systems are possible. Once again, overall requirements for the design and security of the system and its annal will vary and must part under ethical and legal principles specific to the time and place.[ citation needed ]
While it is currently unknown precisely how long EHRs volition be preserved, information technology is certain that length of time volition exceed the boilerplate shelf-life of newspaper records. The development of applied science is such that the programs and systems used to input information will probable not be available to a user who desires to examine archived data. Ane proposed solution to the challenge of long-term accessibility and usability of data by future systems is to standardize information fields in a time-invariant fashion, such every bit with XML language. Olhede and Peterson report that "the bones XML-format has undergone preliminary testing in Europe by a Spri project and been found suitable for EU purposes. Spri has advised the Swedish National Board of Health and Welfare and the Swedish National Archive to issue directives concerning the utilize of XML equally the archive-format for EHCR (Electronic Health Care Record) data."[110]
Synchronization of records [edit]
When care is provided at 2 different facilities, it may exist hard to update records at both locations in a co-ordinated fashion. Two models have been used to satisfy this problem: a centralized data server solution, and a peer-to-peer file synchronization program (equally has been adult for other peer-to-peer networks). Synchronization programs for distributed storage models, however, are only useful once record standardization has occurred. Merging of already existing public healthcare databases is a common software challenge. The ability of electronic health tape systems to provide this function is a key benefit and can improve healthcare delivery.[111] [112] [113]
eHealth and teleradiology [edit]
The sharing of patient information between wellness care organizations and Information technology systems is irresolute from a "bespeak to point" model to a "many to many" one. The European Committee is supporting moves to facilitate cross-border interoperability of due east-wellness systems and to remove potential legal hurdles, as in the projection world wide web.epsos.european union/. To allow for global shared workflow, studies will exist locked when they are being read then unlocked and updated once reading is consummate. Radiologists will be able to serve multiple wellness intendance facilities and read and report beyond big geographical areas, thus balancing workloads. The biggest challenges will chronicle to interoperability and legal clarity. In some countries it is almost forbidden to practise teleradiology. The multifariousness of languages spoken is a problem and multilingual reporting templates for all anatomical regions are non yet available. However, the marketplace for e-health and teleradiology is evolving more rapidly than any laws or regulations.[114]
Russia [edit]
In 2011, Moscow's government launched a major project known as UMIAS every bit role of its electronic healthcare initiative. UMIAS - the Unified Medical Information and Belittling Organisation - connects more than 660 clinics and over 23,600 medical practitioners in Moscow. UMIAS covers nine.5 one thousand thousand patients, contains more 359 million patient records and supports more than 500,000 dissimilar transactions daily. Approximately 700,000 Muscovites use remote links to make appointments every calendar week.[115] [116]
European Union: Directive 2011/24/EU on patients' rights in cross-border healthcare [edit]
The European Commission wants to heave the digital economy past enabling all Europeans to have access to online medical records anywhere in Europe past 2020. With the newly enacted Directive 2011/24/Eu on patients' rights in cantankerous-border healthcare due for implementation by 2013, it is inevitable that a centralised European health tape organization will become a reality even earlier 2020. All the same, the concept of a centralised supranational central server raises business about storing electronic medical records in a cardinal location. The privacy threat posed by a supranational network is a key concern. Cross-edge and Interoperable electronic health record systems make confidential information more easily and chop-chop accessible to a wider audience and increase the risk that personal data concerning health could be accidentally exposed or easily distributed to unauthorised parties by enabling greater access to a compilation of the personal data concerning health, from different sources, and throughout a lifetime.[117]
In veterinary medicine [edit]
In Britain veterinary practice, the replacement of paper recording systems with electronic methods of storing animal patient information escalated from the 1980s and the majority of clinics now utilise electronic medical records. In a sample of 129 veterinary practices, 89% used a Practise Management System (PMS) for information recording.[118] There are more than ten PMS providers currently in the UK. Collecting data straight from PMSs for epidemiological analysis abolishes the demand for veterinarians to manually submit individual reports per animal visit and therefore increases the reporting rate.[119]
Veterinary electronic medical record data are existence used to investigate antimicrobial efficacy; risk factors for canine cancer; and inherited diseases in dogs and cats, in the modest animal disease surveillance project 'VetCOMPASS' (Veterinary Companion Brute Surveillance System) at the Royal Veterinary Higher, London, in collaboration with the University of Sydney (the VetCOMPASS projection was formerly known as VEctAR).[120] [121]
Turing exam [edit]
A letter published in Communications of the ACM[122] describes the concept of generating synthetic patient population and proposes a variation of Turing test to assess the departure between synthetic and real patients. The alphabetic character states: "In the EHR context, though a human physician tin can readily distinguish betwixt synthetically generated and real live human patients, could a machine exist given the intelligence to brand such a determination on its own?" and farther the alphabetic character states: "Earlier synthetic patient identities become a public wellness trouble, the legitimate EHR market place might benefit from applying Turing Test-similar techniques to ensure greater data reliability and diagnostic value. Any new techniques must thus consider patients' heterogeneity and are probable to have greater complexity than the Allen eighth-grade-science-test is able to grade."[123]
See also [edit]
- Electronic health records in the Usa
- Electronic health records in England
- Clinical documentation improvement
- European Institute for Health Records (EuroRec)
- Health informatics
- Health information management
- Health information technology
- Health Information Technology for Economic and Clinical Health Human activity
- Hospital information system
- List of open-source wellness software
- Masking (Electronic Health Record)
- Medical imaging
- Medical privacy
- Medical tape
- Personal wellness record
- Personally Controlled Electronic Health Record, the Australian government's shared electronic health summary system[124]
- Moving picture archiving and communication arrangement
- Radiological information system
- Solid wellness[125]
References [edit]
- ^ Gunter, Tracy D; Terry, Nicolas P (March 2005). "The emergence of national electronic health tape architectures in the The states and Australia: models, costs, and questions". Journal of Medical Internet Research. vii (1): e3. doi:10.2196/jmir.7.1.e3. PMC1550638. PMID 15829475.
- ^ "Mobile Tech Contributions to Healthcare and Patient Feel". Tiptop Mobile Trends. 22 May 2014. Archived from the original on 30 May 2014. Retrieved 29 May 2014.
- ^ Chris Kimble (2014). "Electronic Wellness Records: Cure-All or Chronic Condition?". Global Business and Organizational Excellence. 33 (4): 63–74. arXiv:1405.2088. doi:ten.1002/JOE.21554. ISSN 1932-2054. Wikidata Q59454975.
- ^ Cowie, Martin; Blomster, Juuso; Curtis, Lesley; Duclaux, Sylvie; Ford, Ian; Fritz, Fleur; Goldman, Samantha; Janmohamed, Salim; Kreuzer, Jorg; Leenay, Mark; Michel, Alexander; Ong, Seleen; Pell, Jill; Southworth, Mary Ross; Stough, Wendy Gattis; Thoenes, Martin; Zannad, Faiez; Zalewski, Andrew (2017). "Electronic health records to facilitate clinical research". United states of america National Library of Medication. 106 (one): i–9. doi:x.1007/s00392-016-1025-6. PMC5226988. PMID 27557678.
- ^ Cowie, Martin; Blomster, Juuso; Curtis, Lesley; Duclaux, Sylvie; Ford, Ian; Frtiz, Fleur; Goldman, Samantha; Janmohamed, Salim; Kreuzer, Jorg; Leenay, Marking; Michel, Alexander; Ong, Seleen; Pell, Jill; Southworth, Mary Ross; Stough, Wendy Gattis; Thoenes, Martin; Zannad, Faiez; Zalewski, Andrew (2016). "Electronic wellness records to facilitate clinical research". United states of america National Library of Medication. 106 (ane): 1–9. doi:x.1007/s00392-016-1025-6. PMC5226988. PMID 27557678.
- ^ a b c "What are the advantages of electronic wellness records?". Wellness It.
- ^ Habib JL (2010). "EHRs, meaningful use, and a model EMR". Drug Benefit Trends. 22 (iv): 99–101.
- ^ Kierkegaard P (2011). "Electronic health tape: Wiring Europe's healthcare". Estimator Law & Security Review. 27 (5): 503–515. doi:10.1016/j.clsr.2011.07.013.
- ^ "What is a personal health record?". HealthIT.gov. Office of the National Coordinator for Wellness Information technology. Archived from the original on 25 July 2015. Retrieved 24 July 2015.
- ^ a b c Greenhalgh T, Potts HWW, Wong G, Bark P, Swinglehurst D (2009). "Tensions and paradoxes in electronic patient record research: A systematic literature review using the meta-narrative method". Milbank Quarterly. 87 (four): 729–88. doi:10.1111/j.1468-0009.2009.00578.ten. PMC2888022. PMID 20021585.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Griffin Hospital reports of dozens of patient medical records breaches", CtPost.com, 29 March 2010
- ^ Kate Ramunni; "UCLA hospital scandal grows" Los Angeles Times, 5 August 2008
- ^ Ozair, Fouzia; Jamshed, Nayer; Sharma, Amit; Aggarwal, Praveen (April–June 2015). "Ethical issues in electronic health records: A full general overview". Perspectives in Clinical Research. 6 (2): 73–76. doi:ten.4103/2229-3485.153997. PMC4394583. PMID 25878950.
- ^ Found of Medicine (1999). "To Err Is Human: Building a Safer Wellness System (1999)" (PDF). The National Academies Press. Retrieved 28 Feb 2017.
{{cite spider web}}: CS1 maint: uses authors parameter (link) - ^ Abha, Agarwal (June 2009). "Medication errors: prevention using data applied science systems". British Periodical of Clinical Pharmacology. 67 (half-dozen): 681–686. doi:10.1111/j.1365-2125.2009.03427.10. PMC2723209. PMID 19594538.
- ^ "Electronic Health Record Mistake Prevention Arroyo Using Ontology in Big Data" (PDF). 2015 IEEE 17th International Conference on Loftier Performance and Communications (HPCC). 2015.
- ^ "EMR Software Information Exchange, January 25, 2011". EMR Software Pro. 2011. Archived from the original on two January 2020. Retrieved 3 August 2013.
- ^ "Wellness Information Exchanges and Your EMR Selection Process", New England Journal of Medicine, 25 January 2011
- ^ "Clinical Data Technologies and Inpatient Outcomes". Medical Benefits. 26: half-dozen, 8. thirty March 2009. ProQuest 207235826.
- ^ Adapted from the IEEE definition of interoperability, and legal definitions used by the FCC (47 CFR 51.3), in statutes regarding copyright protection (17 USC 1201), and e-regime services (44 USC 3601)
- ^ "EHR Definition, Attributes and Essential Requirements" (PDF). Healthcare Information and Direction Systems Society. 2003. Archived from the original (PDF) on xix May 2006. Retrieved 28 July 2006.
152 KiB
- ^ Christopher JL Murray; et al. (12 February 2022). "Global burden of bacterial antimicrobial resistance in 2019: a systematic assay". The Lancet. 399 (10325): 629–655. doi:x.1016/S0140-6736(21)02724-0. ISSN 0140-6736. PMC8841637. PMID 35065702.
- ^ Solomon, Daniel H.; Liu, Chih-Chin; Kuo, I.-Hsin; Zak, Agnes; Kim, Seoyoung C. (ane September 2016). "Furnishings of colchicine on hazard of cardiovascular events and mortality among patients with gout: a cohort written report using electronic medical records linked with Medicare claims". Annals of the Rheumatic Diseases. 75 (9): 1674–1679. doi:10.1136/annrheumdis-2015-207984. ISSN 0003-4967. PMC5049504. PMID 26582823.
- ^ Newschaffer, Craig J.; Bush, Trudy L.; Penberthy, Lynne T. (i June 1997). "Comorbidity measurement in elderly female person breast cancer patients with administrative and medical records data". Journal of Clinical Epidemiology. fifty (six): 725–733. doi:10.1016/S0895-4356(97)00050-4. ISSN 0895-4356. PMID 9250271.
- ^ Byun, Jinyoung; Schwartz, Ann K; Lusk, Christine; Wenzlaff, Angela Southward; de Andrade, Mariza; Mandal, Diptasri; Gaba, Colette; Yang, Ping; You, Ming; Kupert, Elena Y; Anderson, Marshall W; Han, Younghun; Li, Yafang; Qian, David; Stilp, Adrienne; Laurie, Cathy; Nelson, Sarah; Zheng, Wenying; Hung, Rayjean J; Gaborieau, Valerie; Mckay, James; Brennan, Paul; Caporaso, Neil East; Landi, Maria Teresa; Wu, Xifeng; McLaughlin, John R; Brhane, Yonathan; Bossé, Yohan; Pinney, Susan M; Bailey-Wilson, Joan Due east; Amos, Christopher I (21 September 2018). "Genome-wide association written report of familial lung cancer". Carcinogenesis. 39 (nine): 1135–1140. doi:ten.1093/carcin/bgy080. PMC6148967. PMID 29924316.
- ^ a b Loukides, Grigorios; Gkoulalas-Divanis, Aris; Malin, Bradley (27 April 2010). "Anonymization of electronic medical records for validating genome-wide association studies". Proceedings of the National Academy of Sciences. 107 (17): 7898–7903. Bibcode:2010PNAS..107.7898L. doi:10.1073/pnas.0911686107. ISSN 0027-8424. PMC2867915. PMID 20385806.
- ^ Al-Zubaidie, Mishall; Zhang, Zhongwei; Zhang, Ji (January 2019). "PAX: Using Pseudonymization and Anonymization to Protect Patients' Identities and Data in the Healthcare System". International Journal of Environmental Enquiry and Public Health. 16 (9): 1490. doi:10.3390/ijerph16091490. ISSN 1660-4601. PMC6540163. PMID 31035551.
- ^ Tamersoy, Acar; Loukides, Grigorios; Nergiz, Mehmet Ercan; Saygin, Yucel; Malin, Bradley (May 2012). "Anonymization of Longitudinal Electronic Medical Records". IEEE Transactions on Information technology in Biomedicine. sixteen (3): 413–423. doi:10.1109/TITB.2012.2185850. ISSN 1558-0032. PMC3779068. PMID 22287248.
- ^ Chevrier, Raphaël; Foufi, Vasiliki; Gaudet-Blavignac, Christophe; Robert, Arnaud; Lovis, Christian (31 May 2019). "Use and Understanding of Anonymization and De-Identification in the Biomedical Literature: Scoping Review". Journal of Medical Internet Enquiry. 21 (five): e13484. doi:10.2196/13484. PMC6658290. PMID 31152528.
- ^ Puri, Vartika; Sachdeva, Shelly; Kaur, Parmeet (one May 2019). "Privacy preserving publication of relational and transaction data: Survey on the anonymization of patient data". Computer science Review. 32: 45–61. doi:10.1016/j.cosrev.2019.02.001. ISSN 1574-0137. S2CID 133142770.
- ^ Falcón, Luis (nine Apr 2020). "Tackling the creature: Using GNU Health to help the fight against the | Joinup". joinup.ec.europa.eu . Retrieved 8 April 2021.
- ^ EMR in Ambulances, "Emergency Medical Paramedic", 5 May 2011. Retrieved 4 June 2011.
- ^ Porter A, Badshah A, Blackness South, Fitzpatrick D, Harris-Mayes R, Islam S, Jones Grand, Kingston K, LaFlamme-Williams Y, Stonemason S, McNee Thou, Morgan H, Morrison Z, Mountain P, Potts H, Rees N, Shaw D, Siriwardena N, Snooks H, Spaight R, Williams Five (2020). Electronic wellness records in ambulances: the ERA multiple-methods study. Health Services and Delivery Research, 8(10). doi:10.3310/hsdr08100
- ^ "NEMSIS - National Ems Data System". nemsis.org. Archived from the original on 8 June 2017. Retrieved 31 May 2017.
- ^ Ambulance Victoria Annual Report Archived 20 July 2011 at the Wayback Automobile, "Ambulance Victoria", 4 Oct 2009. Retrieved 4 June 2011.
- ^ "Electronic Health Records: What's in it for Everyone?". Cdc.gov. 26 July 2011. Archived from the original on ane April 2013. Retrieved 4 September 2013.
- ^ "Handwriting and mobile computing experts". Medscribbler. Scriptnetics. Archived from the original on xix September 2008. Retrieved 20 August 2008.
- ^ "M958 revision-Outcome monitors in PHS 1-02-02.PDF" (PDF). Archived from the original (PDF) on 27 February 2012. Retrieved three August 2013.
- ^ Herwehe J, Wilbright W, Abrams A, Bergson S, Foxhood J, Kaiser Yard, Smith L, Xiao Thou, Zapata A, Magnus Thou (2011). "Implementation of an innovative, integrated electronic medical record (EMR) and public wellness information substitution for HIV/AIDS". Journal of the American Medical Informatics Association. 19 (3): 448–52. doi:10.1136/amiajnl-2011-000412. PMC3341789. PMID 22037891.
- ^ a b Greenhalgh T, Potts HW, Wong G, Bark P, Swinglehurst D (December 2009). "Tensions and paradoxes in electronic patient tape inquiry: a systematic literature review using the meta-narrative method". The Milbank Quarterly. 87 (4): 729–88. doi:x.1111/j.1468-0009.2009.00578.x. PMC2888022. PMID 20021585.
- ^ Berg M (1997). "Of Forms, Containers, and the Electronic Medical Record: Some Tools for a Sociology of the Formal". Science, Technology, & Human Values. 22 (4): 403–433. doi:10.1177/016224399702200401. S2CID 109278148.
- ^ Greenhalgh T, Stramer Thou, Bratan T, Byrne E, Russell J, Potts HW (June 2010). "Adoption and non-adoption of a shared electronic summary record in England: a mixed-method case study". BMJ. 340: c3111. doi:ten.1136/bmj.c3111. PMID 20554687.
- ^ Gabriel B (2008). "Do EMRs Make You a Ameliorate Doctor?". Physicians Practice. Archived from the original on eight June 2010. Retrieved 23 August 2009.
- ^ Electronic health records not a panacea
- ^ Silverstein South (2009). "2009 a pivotal twelvemonth in healthcare IT". Drexel University. Archived from the original on 10 December 2010. Retrieved five Jan 2010.
- ^ a b Himmelstein DU, Wright A, Woolhandler Southward (January 2010). "Hospital calculating and the costs and quality of intendance: a national report". The American Journal of Medicine. 123 (i): twoscore–six. CiteSeerX10.i.1.176.937. doi:10.1016/j.amjmed.2009.09.004. PMID 19939343.
- ^ Cebul RD, Honey TE, Jain AK, Hebert CJ (September 2011). "Electronic wellness records and quality of diabetes care". The New England Journal of Medicine. 365 (9): 825–33. doi:x.1056/NEJMsa1102519. PMID 21879900.
- ^ "Improve Intendance Coordination using Electronic Health Records | Providers & Professionals". HealthIT.gov. Retrieved iv September 2013.
- ^ "Principal Care Patients Utilise Interactive Preventive Health Record Integrated With Electronic Health Record, Leading to Enhanced Provision of Preventive Services". Agency for Healthcare Research and Quality. xix June 2013. Retrieved nine July 2013.
- ^ a b RWIF, GWUMC, IHP Staff (2006). "Health It in the United states: The Data Base for Progress" (PDF). Robert Woods Johnson Foundation, George Washington University Medical Centre, and Institute for Health Policy. Archived from the original (PDF) on 17 May 2008. Retrieved 17 February 2008.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Evidence on the costs and benefits of wellness data engineering. Congressional Budget Office, May 2008.
- ^ Shah Due south. "Column: Why MDs Dread EMRs". Journal of Surgical Radiology. Archived from the original on 10 September 2012.
- ^ It: Not a Cure for the High Cost of Health Care. Knowledge@Wharton, June 10, 2009.[1]
- ^ Abraham Verghese. The Myth of Prevention. The Wall Street Periodical, June twenty, 2009.[2]
- ^ Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG (May 2006). "Systematic review: affect of health information engineering on quality, efficiency, and costs of medical care". Annals of Internal Medicine. 144 (10): 742–52. doi:10.7326/0003-4819-144-10-200605160-00125. PMID 16702590.
- ^ "7 big reasons why EHRs consume physicians' days and nights". The American Medical Association.
- ^ Defining and Testing EMR Usability. Healthcare Data and Management Systems Gild, June 2009.[3] Archived 22 March 2012 at the Wayback Machine
- ^ NISTIR 7804: Technical Evaluation, Testing and Validation of the Usability of Electronic Health Records, p. 9–10. National Plant of Standards and Engineering science, Sept. 2011.[4]
- ^ "U.S. Medicine – The Vocalism of Federal Medicine, May 2009.". Archived from the original on 7 Oct 2011. Retrieved 27 January 2012.
- ^ Bouamrane, Matt-Mouley; Mair, Frances S. (2013). "A Report of General Practitioners' Perspectives on Electronic Medical Records Systems in NHSScotland". BMC Medical Informatics and Decision Making. thirteen: 58. doi:10.1186/1472-6947-13-58. PMC3704757. PMID 23688255.
- ^ Fiks AG, Alessandrini EA, Forrest CB, Khan Due south, Localio AR, Gerber A (2011). "Electronic medical tape utilise in pediatric primary care". Periodical of the American Medical Informatics Association. 18 (1): 38–44. doi:10.1136/jamia.2010.004135. PMC3005866. PMID 21134975.
- ^ "EHRs Go Mobile" Archived x September 2012 at the Wayback Motorcar Marisa Torrieri, Physicians Practice, July/August 2012.
- ^ Turchin, Alexander; Florez Builes, Luisa F. (19 March 2021). "Using Natural Language Processing to Measure and Ameliorate Quality of Diabetes Care: A Systematic Review". Journal of Diabetes Science and Technology. 15 (3): 553–560. doi:ten.1177/19322968211000831. ISSN 1932-2968. PMC8120048. PMID 33736486.
- ^ Wanyan, Tingyi; Honarvar, Hossein; Azad, Ariful; Ding, Ying; Glicksberg, Benjamin South. (8 September 2021). "Deep Learning with Heterogeneous Graph Embeddings for Mortality Prediction from Electronic Health Records". Data Intelligence. 3 (iii): 329–339. arXiv:2012.14065. doi:10.1162/dint_a_00097. ISSN 2641-435X. S2CID 229679954.
- ^ Granja C, Janssen W, Johansen MA (May 2018). "Factors Determining the Success and Failure of eHealth Interventions: Systematic Review of the Literature". Journal of Medical Internet Research. 20 (5): e10235. doi:10.2196/10235. PMC5954232. PMID 29716883.
- ^ Kling, Rosenbaum, Sawyer, Indiana Academy. Understanding And Communicating Social Informatics: A Framework For Studying And Pedagogy The Human Contexts of Information And Communication Technologies, pg. 23. Data Today Inc (xv September 2005), ISBN 978-1-57387-228-vii
- ^ Sawyer and Rosenbaum. Social Informatics in the Information Sciences: Electric current Activities and Emerging Directions, p. 94.Informing Science: Special Issue on Information Science Research, Vol. 3 No. 2, 2000.[5]
- ^ Tenner, Edward. Why Things Bite Back: Technology and the Revenge of Unintended Consequences. ISBN 978-0-679-74756-7, 1997.
- ^ United states Joint Commission on Accreditation of Healthcare Organizations (December 2008). "Safely implementing wellness information and converging technologies". Sentinel Event Alert (42): 1–4. PMID 19108351.
- ^ MEDMARX Agin Drug Result Reporting database
- ^ Wellness informatics – Guidance on the management of clinical gamble relating to the deployment and use of health software (formerly ISO/TR 29322:2008(East)). DSCN18/2009, Examples of potential harm presented by health software, Annex A, p. 38 [half-dozen] Archived 15 July 2014 at the Wayback Machine.
- ^ FDA memo. H-IT Prophylactic Bug, tabular array 4, folio 3, Appendix B, p. 7–viii (with examples), and p. v, summary. Memo obtained and released by Fred Schulte and Emma Schwartz at the Huffington Post Investigative Fund, now part of the Center for Public Integrity, in a 3 August 2010 article FDA, Obama digital medical records team at odds over safety oversight[7] Archived 2 April 2015 at the Wayback Machine, memo itself [8] Archived half-dozen September 2015 at the Wayback Machine
- ^ Goodman KW, Berner ES, Dente MA, Kaplan B, Koppel R, Rucker D, Sands DZ, Winkelstein P (2010). "Challenges in ideals, safety, best practices, and oversight regarding HIT vendors, their customers, and patients: a report of an AMIA special task forcefulness". Periodical of the American Medical Informatics Association. 18 (one): 77–81. doi:ten.1136/jamia.2010.008946. PMC3005880. PMID 21075789.
- ^ Rowe JC. Doctors Get Digital. The New Atlantis (2011).
- ^ Ash JS, Sittig DF, Poon EG, Guappone Yard, Campbell E, Dykstra RH (2007). "The extent and importance of unintended consequences related to computerized provider social club entry". Periodical of the American Medical Computer science Clan. 14 (4): 415–23. doi:ten.1197/jamia.M2373. PMC2244906. PMID 17460127.
- ^ Colligan L, Potts HW, Finn CT, Sinkin RA (July 2015). "Cognitive workload changes for nurses transitioning from a legacy system with newspaper documentation to a commercial electronic health record". International Journal of Medical Informatics. 84 (7): 469–76. doi:10.1016/j.ijmedinf.2015.03.003. PMID 25868807.
- ^ "8 peak challenges and solutions for making EHRs usable". American Medical Clan. sixteen September 2014. Retrieved 12 April 2020.
- ^ Ash, J. S.; Sittig, D. F.; Poon, East. G.; Guappone, K.; Campbell, E.; Dykstra, R. H. (2007). "The Extent and Importance of Unintended Consequences Related to Computerized Provider Order Entry". Journal of the American Medical Informatics Clan. 14 (4): 415–423. doi:ten.1197/jamia.M2373. PMC2244906. PMID 17460127 – via Oxford Academic.
- ^ Evans, R. S. (xx May 2016). "Electronic Wellness Records: Then, Now, and in the Hereafter". Yearbook of Medical Informatics. 25 (Suppl 1): S48–S61. doi:10.15265/IYS-2016-s006. ISSN 0943-4747. PMC5171496. PMID 27199197.
- ^ "Opposition calls for rethink on data storage". due east-Wellness Insider (Britain). Dec 2007. Archived from the original on 7 January 2009.
- ^ "High german doctors say no to centrally stored patient records". e-Health Insider (UK). Jan 2008. Archived from the original on 12 October 2008.
- ^ Fernández-Alemán JL, Sánchez-Henarejos A, Toval A, Sánchez-García AB, Hernández-Hernández I, Fernandez-Luque 50 (June 2015). "Assay of health professional security behaviors in a real clinical setting: an empirical report". International Periodical of Medical Information science. 84 (vi): 454–67. doi:10.1016/j.ijmedinf.2015.01.010. PMID 25678101.
- ^ Wager K, Lee F, Glaser J (2009). Health Care Information Systems: A Practical Approach for Wellness Intendance Direction (2nd ed.). Jossey-Bass. pp. 253–254. ISBN978-0-470-38780-one.
- ^ "Personal Data Protection and Electronic Documents Deed – Implementation Schedule". Office of the Privacy Commissioner of Canada. 1 Apr 2004. Archived from the original on 7 September 2008. Retrieved 12 Feb 2008.
- ^ "Radical relaxation of GP records and booking rules". Health Service Journal. 24 Apr 2020. Retrieved 8 June 2020.
- ^ "Lawyers Per 100,000 Population 1980–2003". Congressional Upkeep Office. Retrieved x July 2007.
- ^ "Tort reform". News Batch. May 2011. Retrieved 4 December 2013.
- ^ "Bigger focus on compliance needed in EMR marketplace". Wellness Imaging News. v Feb 2007. Archived from the original on 29 September 2007.
- ^ "Ben Kerschberg, Electronic Health Records Dramatically Increase Corporate Risk". Huffington Post. 10 January 2010. Retrieved 4 December 2013.
- ^ "Medical Managing director History". Archived from the original on 22 July 2006. Retrieved iv December 2013.
- ^ "Tin Technology Get Yous Sued?" Archived 17 September 2012 at the Wayback Auto Shelly K. Schwartz, Physicians Practice, March 2012.
- ^ Dunlop L (6 April 2007). "Electronic Wellness Records: Interoperability Challenges and Patient's Right for Privacy". Shidler Journal of Reckoner and Engineering 3:16. Archived from the original on 27 October 2007.
- ^ "Newly Issued Last Rules under Stark and Anti-kickback Laws Permit Furnishing of Electronic Prescribing and Electronic Wellness Records Technology". GKLaw. Baronial 2006. Archived from the original on 22 March 2016. Retrieved 30 October 2011.
- ^ "New Stark Law Exceptions and Anti-Kickback Safe Harbors For Electronic Prescribing and Electronic Health Records". SSDlaw. August 2006. Archived from the original on 5 June 2008.
- ^ "epSOS: Legal and Regulatory Issues". Archived from the original on 3 August 2009. Retrieved 4 December 2013.
European Patient Smart Open Services Piece of work Plan
- ^ "Medical Records Manual" (PDF). World Wellness Arrangement. March 2001. Archived from the original (PDF) on 10 July 2012. Retrieved 31 March 2012.
- ^ "ISO/HL7 10781:2009". International Organization for Standardization. Retrieved 31 March 2012.
- ^ Favreau A. "Electronic Principal Intendance Inquiry Network". Regents of the University of Minnesota. Archived from the original on two May 2012. Retrieved 4 Dec 2013.
- ^ a b Kierkegaard P (2012). "Medical information breaches: Notification delayed is notification denied". Figurer Law & Security Review. 28 (two): 163–183. doi:ten.1016/j.clsr.2012.01.003.
- ^ Pear R (thirteen July 2010). "U.Due south. Issues Rules on Electronic Wellness Records". The New York Times.
- ^ "About". smartplatforms.org. Archived from the original on x Apr 2012. Retrieved twenty March 2012.
- ^ Reynolds CL (31 March 2006). "Paper on Concept Processing" (PDF) . Retrieved iv Dec 2013.
- ^ Maekawa Y, Majima Y (2006). "Issues to exist improved after introduction of a non-customized Electronic Medical Record system (EMR) in a Individual General Hospital and efforts toward improvement". Studies in Health Technology and Information science. 122: 919–20. PMID 17102464.
- ^ Tüttelmann F, Luetjens CM, Nieschlag Due east (March 2006). "Optimising workflow in andrology: a new electronic patient record and database". Asian Journal of Andrology. eight (ii): 235–41. doi:x.1111/j.1745-7262.2006.00131.x. PMID 16491277.
- ^ The Digital Office, September 2007, vol 2, no.nine. HIMSS
- ^ Rollins G (2006). "The Perils of Customization". Periodical of AHIMA. 77 (6): 24–28. PMID 16805294.
- ^ Mandl KD, Szolovits P, Kohane IS (February 2001). "Public standards and patients' command: how to keep electronic medical records accessible but individual". BMJ. 322 (7281): 283–7. doi:10.1136/bmj.322.7281.283. PMC1119527. PMID 11157533.
- ^ "Where practise I Find Medical Record Retention Laws for My Land?". Harmony Healthcare IT. February 2020. Archived from the original on xi July 2021. Retrieved 3 September 2021.
- ^ Ruotsalainen P, Manning B (2007). "A notary archive model for secure preservation and distribution of electrically signed patient documents". International Periodical of Medical Informatics. 76 (5–6): 449–53. doi:10.1016/j.ijmedinf.2006.09.011. PMID 17118701.
- ^ Olhede T, Peterson HE (2000). "Archiving of care related information in XML-format". Studies in Health Technology and Informatics. 77: 642–6. PMID 11187632.
- ^ Papadouka V, Schaeffer P, Metroka A, Borthwick A, Tehranifar P, Leighton J, Aponte A, Liao R, Ternier A, Friedman S, Arzt Due north (November 2004). "Integrating the New York citywide immunization registry and the childhood blood lead registry". Journal of Public Health Management and Practice. Suppl: S72–80. CiteSeerXten.1.one.331.2171. doi:10.1097/00124784-200411001-00012. PMID 15643363.
- ^ Gioia PC (2001). "Quality improvement in pediatric well care with an electronic tape". Proceedings. AMIA Symposium: 209–thirteen. PMC2243516. PMID 11825182.
- ^ Williams SD, Hollinshead W (November 2004). "Perspectives on integrated kid wellness information systems: parents, providers, and public wellness". Periodical of Public Wellness Direction and Practice. Suppl: S57–60. doi:ten.1097/00124784-200411001-00009. PMID 15643360.
- ^ Pohjonen H. Images can now cantankerous borders, just what virtually the legislation? Diagnostic Imaging Europe. June/July 2010;26(4):16.
- ^ "CNews: ЕМИАС ограничит количество записей к врачу". gov.cnews.ru. Archived from the original on 31 March 2014. Retrieved 31 March 2014.
- ^ "New programmes and the best doctors, or how Moscow healthcare is being adult / News / Moscow City Web Site".
- ^ Kierkegaard P (2011). "Electronic health record: Wiring Europe's healthcare". Estimator Constabulary & Security Review. 27 (v): 503–515. doi:10.1016/j.clsr.2011.07.013.
- ^ Gill, Thou. (2007) Attitudes to clinical audit in veterinary practice, Royal Veterinary Higher elective project, unpublished piece of work
- ^ Carruthers H (2009). "Disease surveillance in modest animal practice". In Exercise. 31 (7): 356–358. doi:x.1136/inpract.31.7.356. S2CID 71415659.
- ^ "VEctAR (Veterinarian Electronic Animal Record) (2010)". Archived from the original on 28 February 2013.
- ^ Brodbelt D, Midleton S, O'Neil D, Sumers J, Church D (2011). "Companion Animate being Practice Based Disease Surveillance in the UK" (PDF). Épidémiologie et Santé Animale. 59–60: 38–forty.
- ^ Kartoun U (Jan 2018). "A Leap from Bogus to Intelligence". Letters to the editor. Communications of the ACM. 61 (one): x–11. doi:10.1145/3168260.
- ^ Metz, Cade (4 September 2019). "A Breakthrough for A.I. Technology: Passing an 8th-Form Science Test". The New York Times. ISSN 0362-4331. Retrieved 12 May 2021.
- ^ Mendelson D (Baronial 2004). "HealthConnect and the duty of care: a dilemma for medical practitioners". Journal of Law and Medicine. 12 (1): 69–79. PMID 15359551.
- ^ Investigating Decentralized Management of Health and Fitness Data
External links [edit]
- Tin can Electronic Health Record Systems Transform Health Care?
- Open up-Source EHR Systems for Ambulatory Care: A Market Cess (California HealthCare Foundation, January 2008)
- US Section of Health and Human Services (HHS), Office of the National Coordinator for Health Information technology (ONC)
- US Section of Health and Human Services (HHS), Agency for Healthcare Enquiry and Quality (AHRQ), National Resource Centre for Wellness Information technology
- Security Aspects in Electronic Personal Health Tape: Information Access and Preservation – a conference newspaper at Digital Preservation Europe
What Parameter Does An Ehr Consider To Find Information On Service-specific Data?,
Source: https://en.wikipedia.org/wiki/Electronic_health_record
Posted by: fishervered1989.blogspot.com


0 Response to "What Parameter Does An Ehr Consider To Find Information On Service-specific Data?"
Post a Comment